To help prevent bleeding, people with hemophilia can be given infusions (injections directly into the blood) of the clotting factor they lack. Your child’s doctor will determine which clotting factor they are missing and determine if factor infusions are appropriate for them. In most cases, this treatment works well. But sometimes, a person’s immune system develops inhibitors, which are antibodies that try to fight the treatment and “inhibit” it from working properly. This is a very serious complication of hemophilia because it means factor replacement therapy is no longer effective. Without treatment, severe internal bleeding can occur. But there are treatments available to help manage inhibitors.
WHO DEVELOPS INHIBITORS, OR ANTIBODIES?
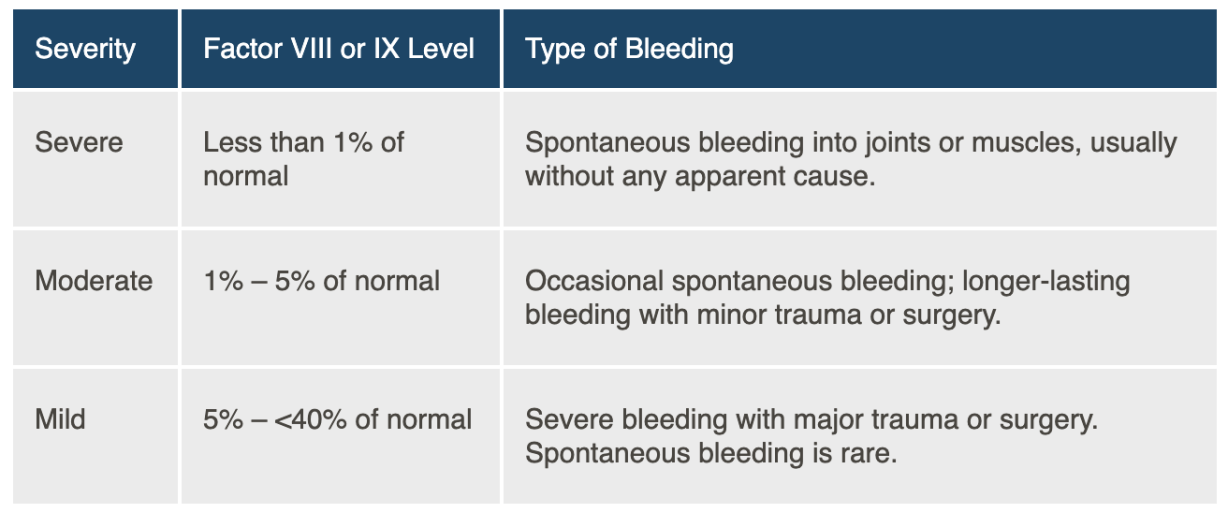
Inhibitors are most common in young children with severe hemophilia A. They usually appear within the first few infusions of Factor VIII therapy. About 1 in 3 of people with severe hemophilia A will develop inhibitors. People with mild to moderate hemophilia A have a lower chance of developing inhibitors – about 1 in 50 – and it usually happens during adulthood. Inhibitors are even more rare in people with hemophilia B (1 in 100), but the complications can be more serious. Other people at a higher risk of developing inhibitors include people:
➥ with a family member with inhibitors
➥ of African descent
Researchers don’t know exactly why some people develop inhibitors, while others do not. People may also have different types of inhibitors: for some, they aren’t very severe and are inactive (have no effect) for periods of time. For others, they are more serious, and don’t go away without effective treatment.
HOW DO YOU KNOW IF SOMEONE HAS DEVELOPED INHIBITORS?
If someone receives an infusion of clotting factor, and they do not respond in the usual way, this could be a sign of inhibitors. For example, a bleed may not properly clot, or it may take 2 or 3 infusions before blood clots properly. A blood test will need to be done to see if inhibitors are present, and treatment can be started as soon as possible to help manage them.
The good news is that in 2 out of 3 cases, inhibitors disappear – either on their own, or after treatment, within 9 months (on average). For others, inhibitors persist and are a serious problem.
TREATING INHIBITORS
Managing inhibitors is complex and one of the biggest challenges facing people with hemophilia. Doctors often treat inhibitors by using something called immune tolerance therapy (ITT), which tries to “teach” the body to stop fighting factor replacement therapy. Very high doses of factor VIII are used in ITT. Sometimes, a doctor will have to try different regimens of ITT to find optimal results. Not everyone will respond to ITT. ITT is usually not effective in people with hemophilia B.
If ITT doesn’t work, other treatment options can be tried. These treatments focus on preventing bleeding, rather than fighting the inhibitors.
COPING WITH INHIBITOR THERAPY
ITT can be very long – up to 3 years – which can be physically and emotionally taxing on a patient and their family. It can be hard to see your child endure more injections. And, it can be frustrating and discouraging: Why did this happen? Why did treatment just ‘stop working? What now?
It’s important to work closely with your healthcare team and your HTC to help get through these challenges. They can help answer your questions and manage expectations. You can’t do everything alone – lean on those around you for support, encouragement and guidance.